How do I submit a pay-direct drug claim?
Most plans offer pay-direct drugs with pharmacies across Canada. Present your drug card to them and they can submit the claim on your behalf—so you don’t have to be out of pocket.
You can now submit drug claims using the new My Claims portal if your plan allows it. If not, please refer to the information below.
Information needed to complete the form
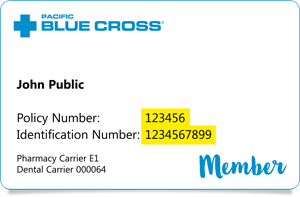
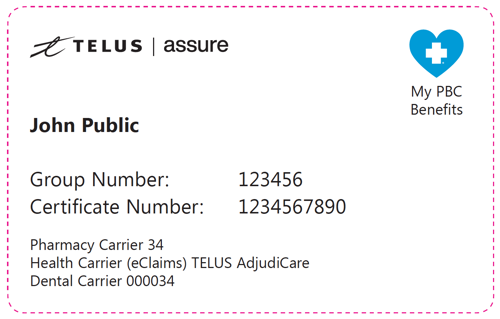
- member I.D. / Certificate Number
- Group policy number
- name of the insured person(s)
- relationship to the employee
- birth date(s)
- Pharmacy Receipt
- original receipts or if you are coordinating claim’s payment with your spouse’s health plan, you should include the primary carrier’s payment statement
- information about other benefit or insurance plans that you may be eligible to claim from.
Steps to complete and submit the form electronically
- Download the Telus Health Solutions (Assure) Drug Claim form.
- Save the downloaded form to your computer.
- Open and complete the form in Adobe Reader. DO NOT complete the form in your browser. Get Adobe Reader from here (it’s free).
- Save changes to your computer, then close and re-open the form to ensure your information was saved.
- Scan or take pictures of your pharmacy receipts and primary carrier’s payment statement.
Note: Our system only permits you to submit 9 receipts per claim! - Email the saved Drug Claim form to health@datownley.com digitally using our secure Mail Express Tool. Here are the instructions on how to use it.
- Copy and save the Mail Express receipt number for your records.
- Do not print and mail the form to our offices.